Fillings
Fillings replace tooth substance lost through various events. The size of the defect is the limiting factor for the various materials that can be used. In addition to the different materials, fillings also differ in their procedures. For example, there are “one-stage” (completed in one appointment) and “two-stage” (requiring two appointments) treatments.
Dental fillings are generally used to repair cavities. However, fillings are also placed to repair small fractures in the tooth structure in order to optimize the function, stability, and aesthetics of teeth.
Material groups for dental fillings
Materials from the following groups are used worldwide for dental fillings:
- Ceramics for inlays and onlays
- Gold alloys for inlays and onlays
- Composites for resin fillings
- Glass ionomer cements
- Compomers
- (Amalgam)
As always in life, there are not only advantages and disadvantages. There are always both. And I will explain these below.
In addition to these materials, there are also newer developments, such as bulk-fill composites that can be applied in thick layers, bioactive filling materials that promote the remineralization of the adjacent tooth structure, and nanohybrid composites with extremely small fillers, which optimize polishability.
Ceramics for inlays and onlays
Ceramic inlays and onlays are high-quality indirect dental fillings that are fabricated outside the mouth (e.g., in a dental laboratory or using CAD/CAM technology) and then bonded into the tooth. They are considered particularly durable and aesthetically pleasing.
The tooth-colored appearance can be perfectly matched to the natural tooth, especially with lithium disilicate or feldspar ceramics. And they do not discolor over time (unlike composites, which can darken with coffee, tea, etc.). Ceramics are inert, meaning there are no known allergies or intolerances. And since ceramics have very poor thermal conductivity, there is hardly any initial temperature sensitivity when using these materials.
Lithium disilicate or zirconium oxide ceramics are very hard and highly break-resistant, allowing them to be used to functionally reinforce even large chewing surfaces. These days, they are usually manufactured digitally, i.e., using CAD/CAM technology, which allows for very high precision. This minimizes the risk of recurrence of caries on the same tooth.
Ceramic inlays and onlays have a lifespan of 10 to 20 years or more, depending on home oral hygiene and professional prophylaxis.
Naturally, this effort entails higher costs. Patients with statutory health insurance (GKV) only receive a subsidy for these inlays and onlays from their insurance for a standard filling, so they must cover a co-payment of €800 to €1,400, depending on the complexity and size.
The indication for ceramic inlays and onlays must be precisely determined, because if the wall thickness is too thin or the load is too uneven, the ceramic can break. This means that such restorations require sufficient residual tooth structure. In addition, the use and correct implementation of the adhesive technique is crucial for longevity.
It is also important to understand that if the ceramic breaks or defects occur, it cannot be repaired, unlike composite fillings, for example. However, it is the best treatment for medium to large defects where composites are contraindicated.
Gold alloys for inlays and onlays
Gold inlays and onlays are among the most durable and proven restorations in restorative dentistry. They are usually made of high-gold alloys and are custom-fabricated in a dental laboratory. This means that this restoration typically requires two appointments.
Gold inlays and onlays are arguably the most durable restorations restorative dentistry has to offer. Their durability is stated to be more than 20 years. My gold inlays lasted more than 45 years. That’s quite a statement!
To achieve such longevity, in addition to good home oral hygiene and excellent professional prophylaxis, excellent skills from both the dentist and the dental technician are required. The fit must be accurate to within a few hundredths of a millimeter. Such precision reduces the risk of marginal caries. There’s no room for compromise!
Another reason for this durability is the minimal malleability of the gold alloy. Through daily chewing, the thin gold edges are imperceptibly adapted to the tooth. This prevents fatigue fractures, even with thin material thicknesses.
High-gold alloys are said to have very good biocompatibility because they hardly cause allergic reactions. However, there are some people who cannot tolerate metal in their mouths. This must be clarified before fabricating high-gold inlays and onlays.
Since gold is a very good conductor of temperature, temperature sensitivity may initially occur after these restorations are inserted. And, of course, gold is gold-colored. These restorations are therefore visible in the front of the mouth. This is important to know!
Given the sharp increase in the price of gold, gold inlays and onlays have also become significantly more expensive. Their costs are higher than those of ceramic inlays and onlays.
Gold inlays and onlays are mechanically unsurpassed when it comes to stability, precision, and durability. They are particularly suitable for patients with high chewing loads, in non-visible areas and for anyone looking for a long-term solution with as little follow-up treatment as possible.
Composite fillings
Composites are one of the most commonly used filling materials in dentistry today, primarily because they are tooth-colored, can be placed directly in the mouth, and are minimally invasive. They consist of a mixture of an organic resin matrix (e.g., Bis-GMA) and inorganic fillers (e.g., glass ceramics, quartz). You can imagine this as tiny grains of sand, which make up approximately 80% of the mass, being bonded together by resin.
A comprehensive assessment must consider not only functional and aesthetic aspects but also potential toxicological risks from components such as bisphenol A (BPA) – see below!
Composite fillings can be easily color-matched to the tooth, but this also requires additional effort and appropriate skills from the dentist and assistant. This material is virtually unbeatable for fillings from “mini” to “midi.” Beyond that, it should be viewed with caution.
A key advantage is that these fillings can be placed in a single appointment. No impression or dental laboratory is required. Modern composites are highly abrasion-resistant. Should minor marginal defects occur over time, these fillings can also be repaired.
And, of course, these fillings are significantly less expensive than ceramic or gold inlays. Depending on the complexity, a certain out-of-pocket cost is charged, ranging from €50 to €150.
But composite fillings also have significant disadvantages. Placing a composite filling is very technique-sensitive. For example, a rubber dam is strongly recommended for absolute dryness. The material also shrinks when light cures, which in turn requires a complex layering technique to compensate for this polymerization shrinkage. Furthermore, composite fillings can become unsightly discolored over time. The overall result can last for approximately five to a sporty ten years. And don’t forget: Composite is not suitable for larger fillings, a fact that is often ignored in German practice, probably for economic reasons.
However, composites do have a certain, albeit low, toxicity and other potential health risks! They contain monomeric components such as bis-GMA (bisphenol A glycidyl methacrylate), UDMA (urethane dimethacrylate), or TEGDMA (triethylene glycol dimethacrylate). After the filling is placed, small amounts of monomers can be released (especially during incomplete polymerization). These substances are suspected of having cytotoxic or endocrine disrupting effects.
Bisphenol A (BPA) is not a direct component of most composites, but can be formed as an impurity or degradation product from bis-GMA. BPA is an endocrine disruptor, meaning it can have hormonal effects (estrogenic effects) in high doses. Studies show that BPA exposure from dental fillings is very low and usually below the toxicological limits. But limits are always a tricky issue… we know!
Composite fillings are a modern, versatile, and aesthetically pleasing solution, especially for small to medium-sized defects. When properly processed, they are considered safe from a health perspective, but for patients with particular sensitivities or during specific life stages (e.g., pregnancy), materials that are as toxicologically safe as possible (e.g., BPA-free composites or glass ionomer cements) should be preferred.
Glass ionomer cement
Glass ionomer cements (GICs) are dental filling materials resulting from the reaction of glass particles (calcium aluminum fluorosilicate glass) with polyalkenoic acids (usually polyacrylic acid). They are primarily used in pediatric dentistry, for temporary fillings, cervical defects, and geriatrics.
Unlike composites, GICs do not contain methacrylate monomers such as Bis-GMA or TEGDMA—which makes them particularly interesting from a toxicological perspective.
GICs are relatively easy to process and exhibit low setting shrinkage. The material is moisture-tolerant, but quite the opposite during the setting phase. GICs adhere to the tooth structure and release fluoride over the long term, which has an anti-cariogenic effect. This makes GICs recommended for children, elderly patients, and patients with dry mouth.
GICs tend to produce unsightly fillings that are dull, opaque, and rough. The material cannot be polished, which can easily lead to discoloration. Plaque also adheres particularly well to this material, which isn’t conducive to prophylaxis.
All in all, you can expect a lifespan of 1 to 5 years for GIC fillings… not exactly outstanding!
Compomere
Compomer fillings are a compromise solution for smaller defects – especially in pediatric dentistry or for patients at high risk of caries who require a certain degree of fluoride effect and ease of application.
From a toxicological point of view, compomers are not completely safe because, like composites, they contain methacrylate-based monomers, including potentially endocrine-disrupting substances. However, their release is minimal when used correctly, which is why they are considered relatively safe. For particularly sensitive groups (e.g., pregnant women or allergy sufferers), GIC or BPA-free composites are often preferable.
Compomers produce acceptable aesthetics, are relatively easy to process, and release fluoride. Although they have better physical properties than GIC, the material is ultimately only suitable for small defects.
Toxicity should not go unmentioned: Like composites, compomers contain monomeric resins that have potentially toxic or endocrine-disrupting properties. This is particularly relevant for Bis-GMA (a degradation product can release bisphenol A (BPA) (estrogen-like effects in high doses)), TEGDMA and HEMA, which are cytotoxic in cell cultures and may cause irritation, and UDMA, which is less toxic than Bis-GMA but potentially cell-damaging in high concentrations. Small amounts of monomers may be released if cured incompletely. When professionally applied and fully polymerized, compomers are considered clinically safe.
Compomer fillings (composite-modified glass ionomer cements) are a hybrid between composite and glass ionomer cement. In my opinion, they combine the disadvantages of GIC with those of composites. This doesn’t make them one of my favorites!
Amalgam – Silver Fillings
Amalgam has been the subject of highly controversial and emotional public debate for decades. Nevertheless, I would like to offer a few points of view to help objectify this discussion.
Since 2018, amalgam has been banned in the EU for children under 15, pregnant women, and breastfeeding women. It has been generally banned in Germany since 2025. An EU-wide ban is planned for 2030.
Amalgam fillings are among the oldest and longest-used materials in dentistry. They consist primarily of a metal powder, usually an alloy of silver, tin, and copper. This powder is mixed at a ratio of approximately 1:1 with elemental mercury (Hg), which binds the metal powder.
Amalgam fillings are cost-effective and can be placed with acceptable results even under adverse conditions. This was the key factor in the long-standing use of this material. The lifespan is stated to be approximately 20 years. However, I have often seen amalgam fillings that were well over 40 years old. The material is very chew-resistant and therefore suitable even for large fillings.
The disadvantages undoubtedly outweigh the advantages, especially the chronic release of mercury, which can lead to gradual mercury poisoning. In addition, amalgam corrodes and can develop cracks in the material and tooth structure. Amalgam releases small amounts of elemental mercury vapor (Hg⁰), especially during fresh placement or removal (grinding, drilling), during heat and chewing stress, and during corrosion from acidic environments. It is important to note that released Hg⁰ is absorbed primarily through the lungs and partially oxidized in the body (Hg²⁺).
Mercury can accumulate in the body, especially in the kidneys, central nervous system, and liver. The half-life is several weeks to months, depending on the organ. Studies have found slightly elevated mercury concentrations in the urine of people with multiple amalgam fillings.
So… that’s it for the topic of amalgam. Now let’s quickly forget about the material!
My final remark
You’ve now seen that the better the fillings should be in all criteria, the higher the technical requirements and thus the overall effort. I think the following strategy is best: select only the filling material that is most suitable, without compromise. And then you should do everything you can to prevent further damage that we have to repair.
So if you want to switch to the winning side, then visit your dentist regularly for preventative care. They will also explain to you your weaknesses when brushing your teeth (dentists have these too!) and what you can do better. And this won’t be explained to you by a health section in the newspaper, but by someone who is very knowledgeable about the subject!
Author: drw
P.S.: When you search the internet for filling materials, it’s quite amusing to see who feels called upon to comment on the topic.
For further information
Here are some links for more information:
https://pubmed.ncbi.nlm.nih.gov/34387873/
https://pubmed.ncbi.nlm.nih.gov/37371625/
These are two ceramic inlays on teeth 46 and 47 (bottom right). I made these inlays in 2008 using CAD/CAM, i.e., in a single session.
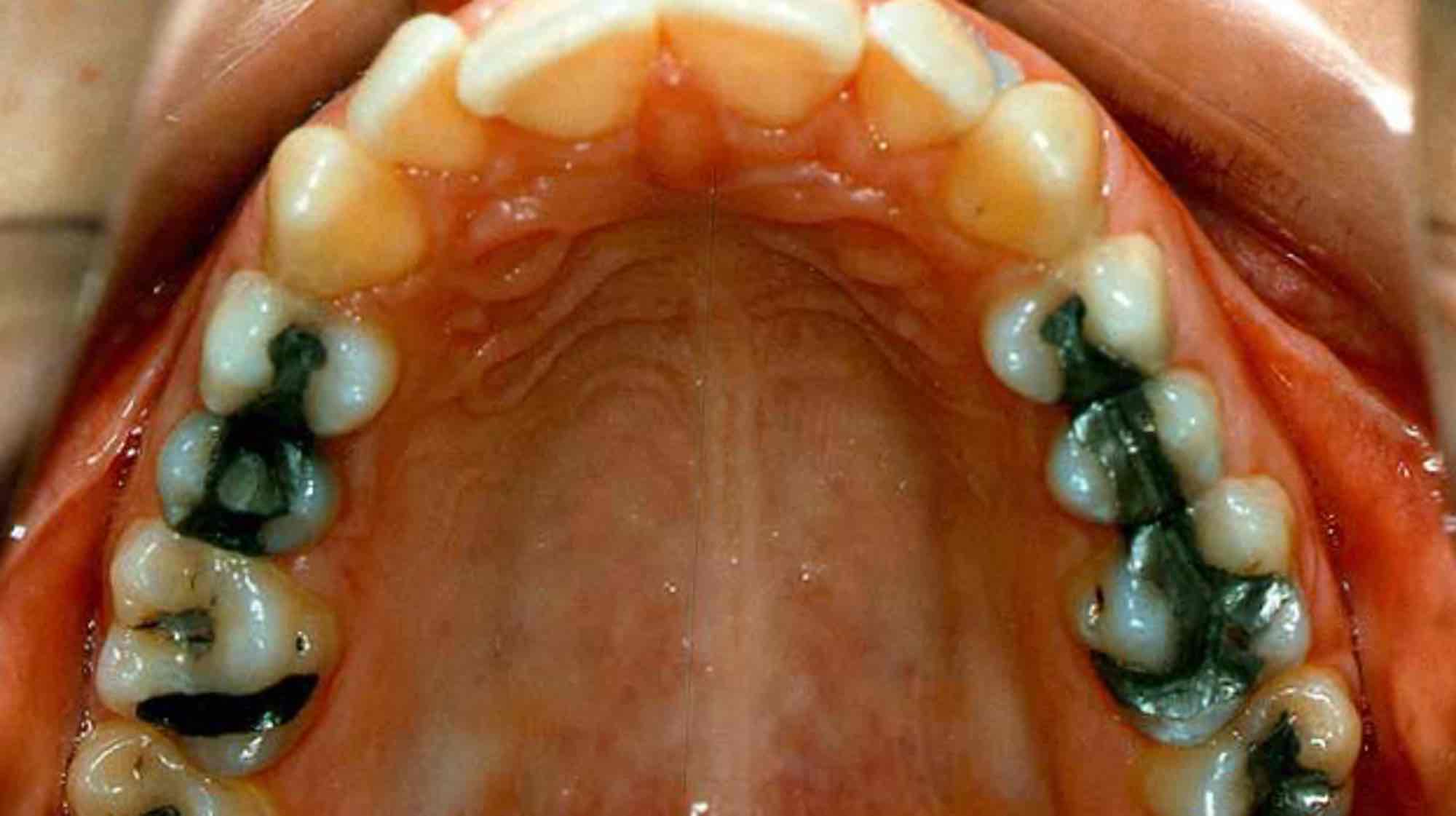
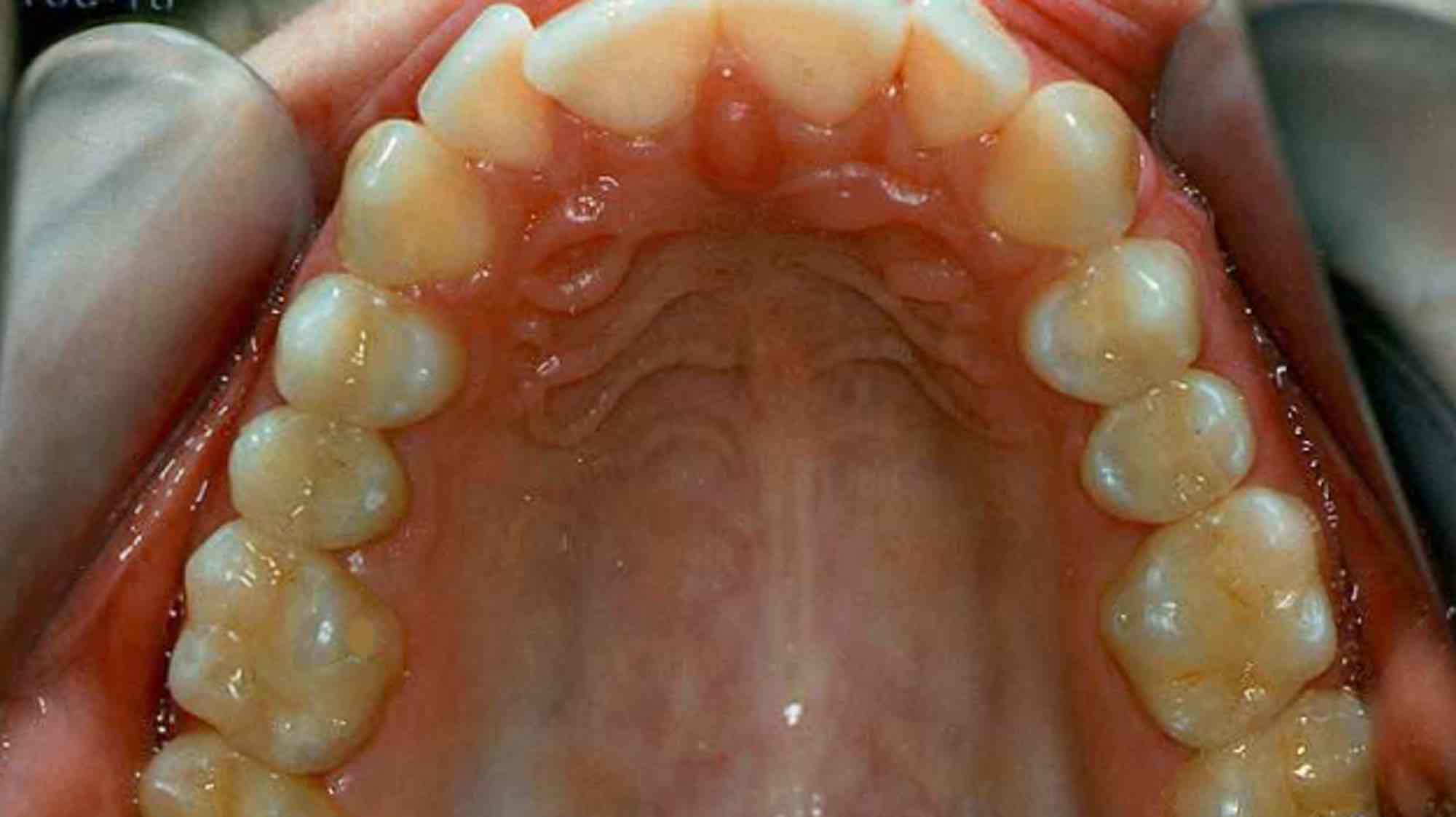
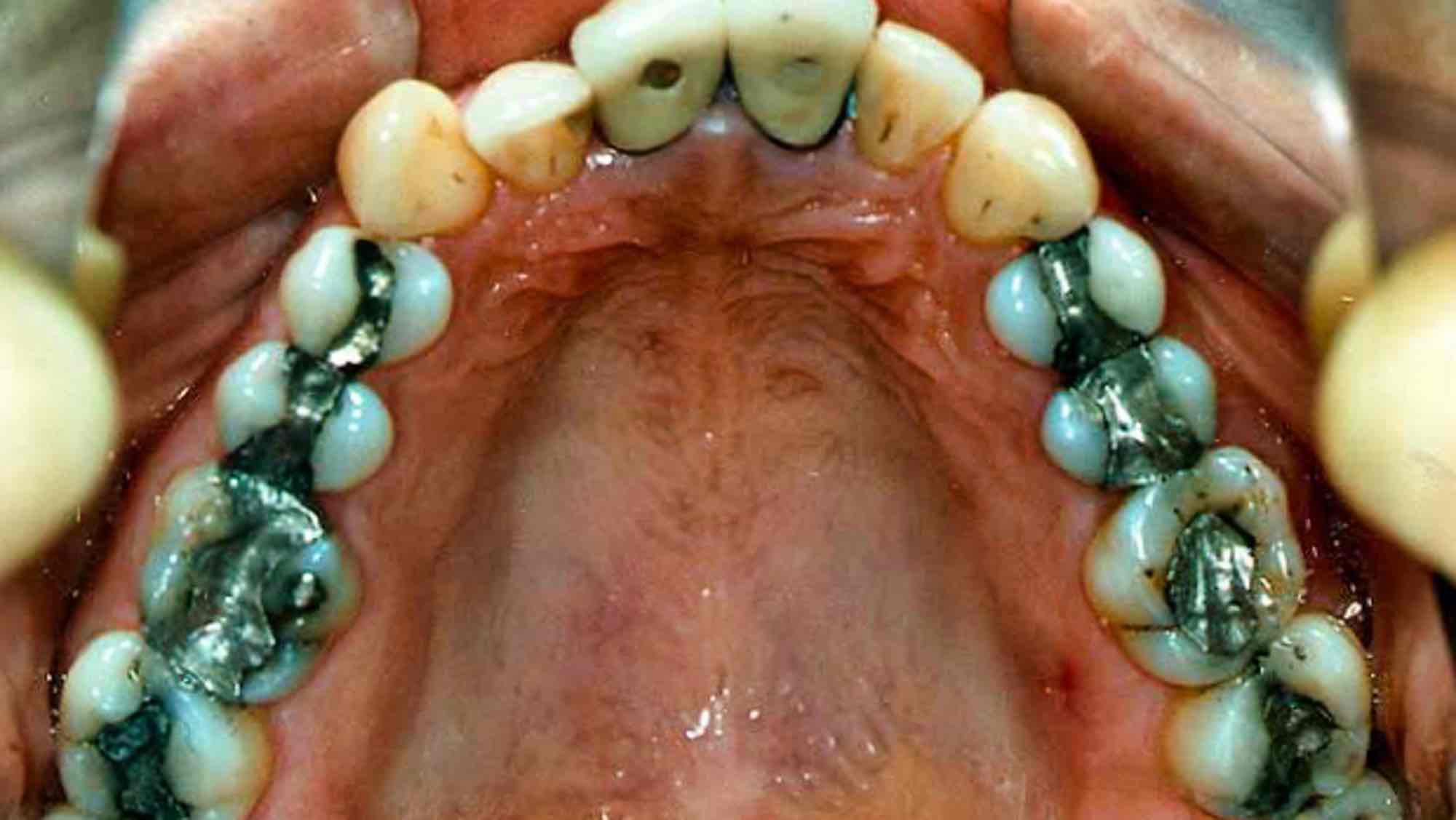
Here is an example of amalgam removal with ceramic inlays and partial crowns.
Two perfect gold inlays!
Here is the before and after of amalgam removal and replacement with gold inlays and gold partial crowns.
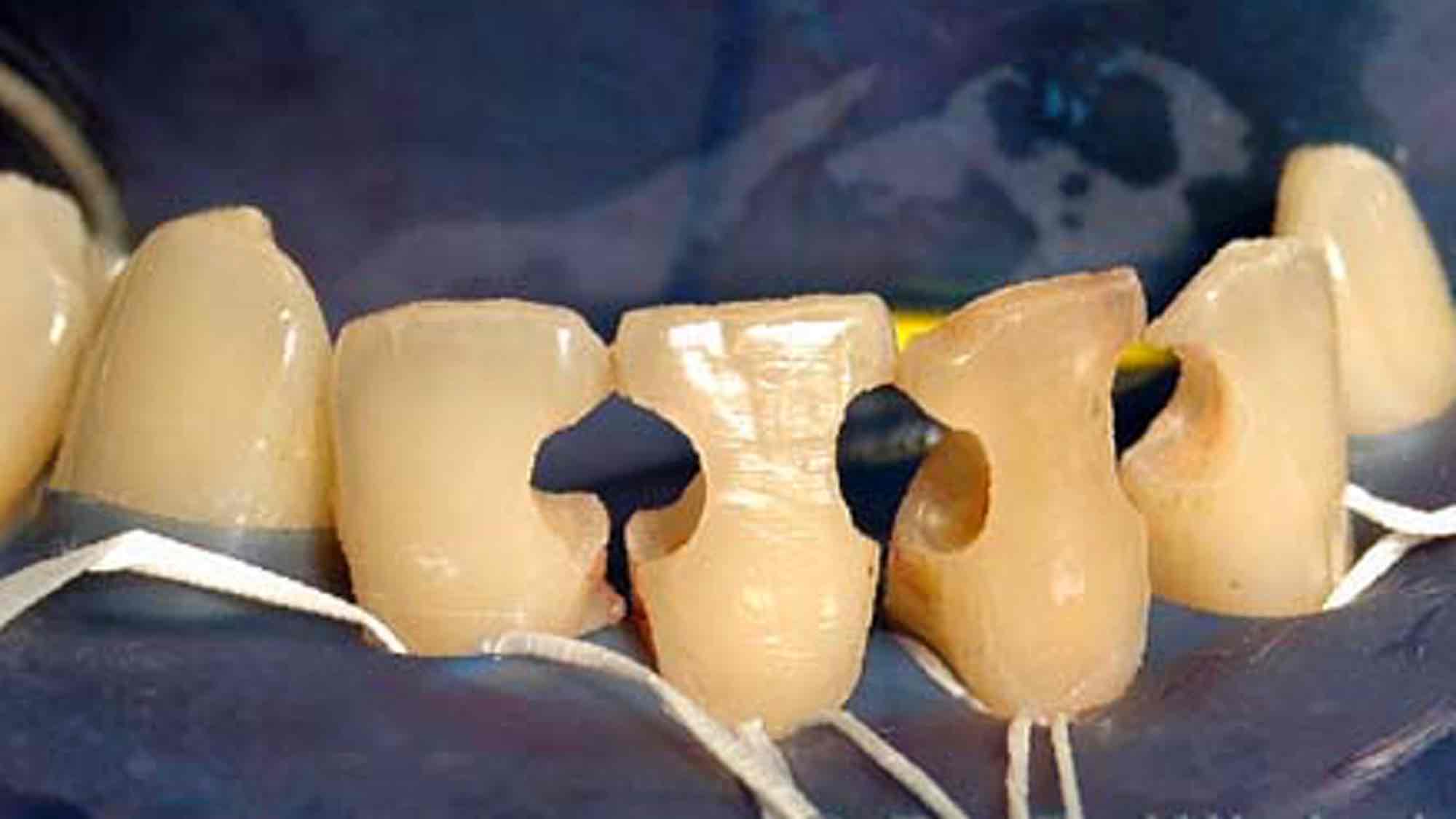
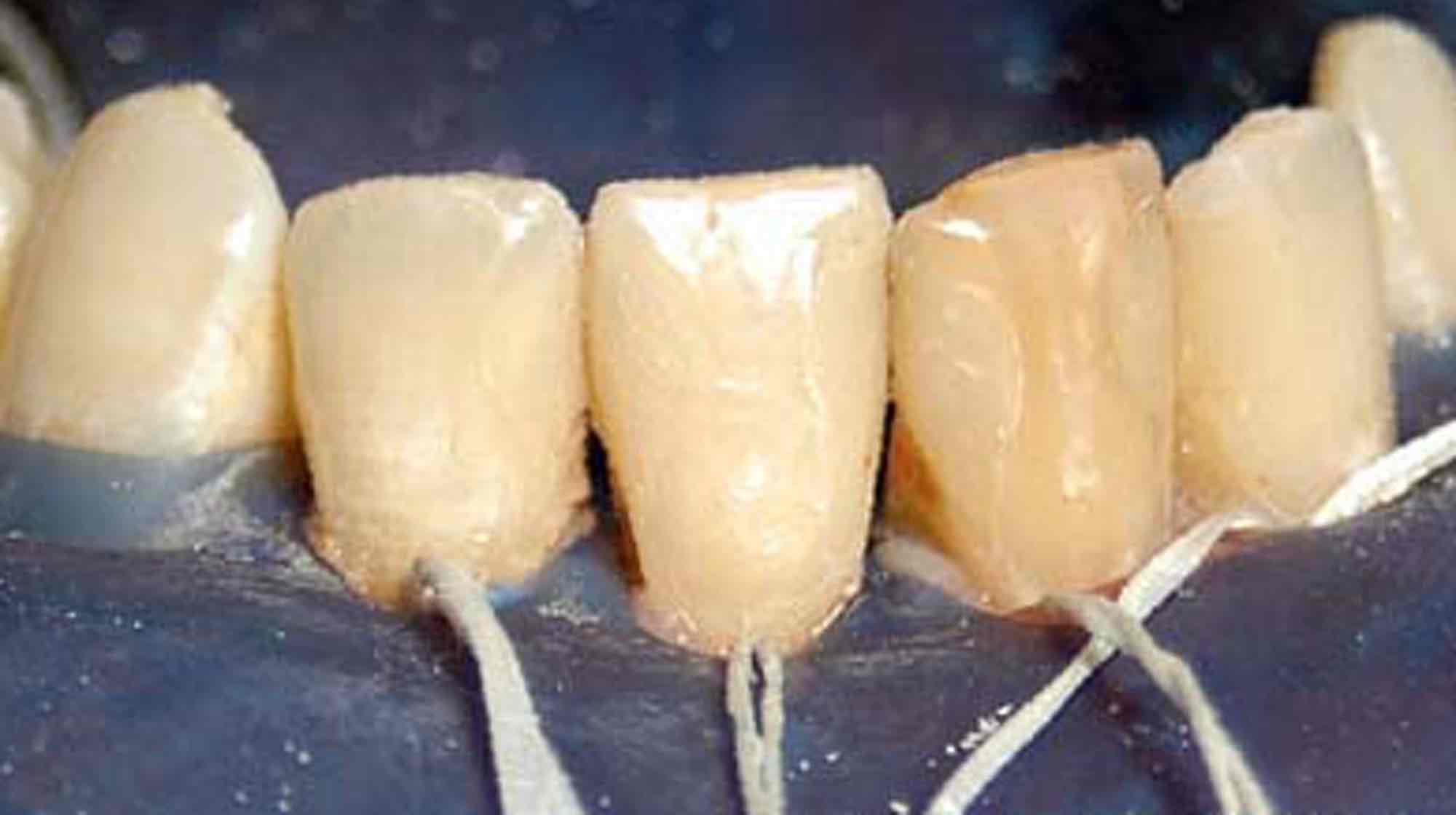
This is what it might look like when composite fillings have to be placed under a rubber dam on upper incisors. These defects are actually much too large for the composite material.
Images of lower incisors. When there are so many “holes” in the anterior lower jaw, we know that the patient’s oral hygiene is extremely poor. These images of a composite restoration under a rubber dam were taken during a treatment under general anesthesia.
Due to trauma (if I remember correctly, it was a water bottle!), the two upper central incisors chipped along the cutting edges. We then repaired it with composite.
Here’s an example of what you can do with composites. Such a structure, of course, requires a tremendous amount of effort, which is ultimately reflected in the costs.
Corroded, broken, marginal cracks, caries at the filling edge… this is what an old amalgam filling looks like.